Candidiasis: Signs, Diagnosis & Treatment
| Test Options |
|
| Treatment | Topical, oral, or intravaginal antifungal medication |
| Price |
|
| Appointment Options |
Same-day appointment (subject to availability). Book via WhatsApp: 8893 3757 or email: hello@healthscreening.sg |
| Clinic Locations |
Orchard: 1 Orchard Blvd
#05-09 Camden Medical Centre, S248649 Tanjong Pagar: 72 Anson Rd #01-02 Anson House, S079911 |
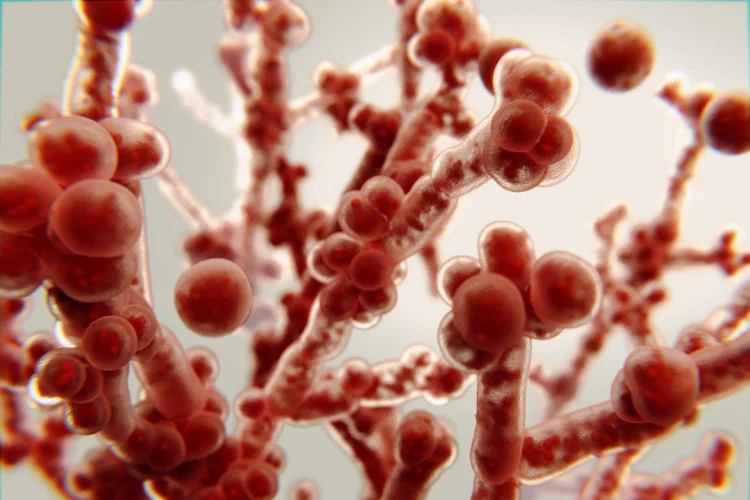
What Is Candidiasis?
Candidiasis refers to a fungal infection caused by yeast belonging to the Candida
genus, most often Candida
albicans. This fungus normally coexists harmlessly on the skin, in the mouth,
gut, and genital tract, but can cause infection when its growth is no longer controlled by the
body’s natural defences. The condition has also been historically called monilia or moniliasis.
In healthy individuals, the immune system and the body’s natural bacteria help maintain the
balance of Candida. However, certain circumstances such as prolonged antibiotic use, diabetes, hormonal changes, or immune
suppression can upset this balance and lead to fungal overgrowth and infection.
Depending on the affected area, candidiasis may cause irritation, soreness, and general
discomfort that can interfere with eating, sleeping, or sexual activity.
What Are Types of Candidiasis and Their Symptoms?
Candidiasis can appear in various forms, each with its own set of symptoms depending on the body site affected. The most common types include vaginal, oral, cutaneous, penile, and invasive candidiasis.
| Type | Description | Symptoms |
|---|---|---|
| Vaginal candidiasis | Occurs when Candida multiplies excessively in the vaginal tract, frequently affecting women during hormonal fluctuations or after antibiotic use. |
|
| Oral candidiasis (thrush) | Affects the mouth and throat, especially in infants, the elderly, or those using inhaled steroids or antibiotics. |
|
| Cutaneous candidiasis | Appears on the skin, often where moisture accumulates such as under the breasts, in the groin, or armpits. |
|
| Penile candidiasis | Affects the head of the penis, particularly in uncircumcised men or those with poor hygiene or diabetes. |
|
| Invasive candidiasis | A severe bloodstream infection that can spread to internal organs, usually occurring in hospitalised or immunocompromised patients. |
|
What Are the Causes of Candidiasis?
Candidiasis develops when the body’s microbial balance is disturbed, allowing Candida to grow unchecked. This imbalance can be triggered by a range of factors:
- Antibiotics – Broad-spectrum antibiotics can kill beneficial bacteria that normally restrict fungal growth.
- Hormonal changes – Pregnancy, oral contraceptives, or hormone therapy may alter vaginal flora and promote fungal proliferation.
- High blood sugar – Poorly managed diabetes increases glucose levels, which can encourage Candida growth.
- Moist environments – Damp or tight clothing and inadequate drying of skin folds create warm, humid conditions ideal for yeast growth.
- Weakened immunity – Illnesses such as HIV, or treatments like chemotherapy or corticosteroids, reduce the body’s resistance to fungal infections.
- Sexual transmission – Although not a sexually transmitted infection (STI), candidiasis can occasionally be transmitted between partners or triggered after sexual contact.
How Is Candidiasis Diagnosed?
Candidiasis is typically diagnosed through a physical examination and laboratory testing, depending on the site and severity of infection.
- Microscopic examination – A swab sample from the affected area may be viewed under a microscope or cultured to confirm the presence of Candida.
- Blood investigations – In suspected systemic (invasive) infection, blood cultures or tests such as β-D-glucan may detect fungal elements circulating in the blood.
- Pelvic assessment – For vaginal symptoms, a pelvic exam and swab test help differentiate candidiasis from other genital infections.

What Is the Treatment for Candidiasis?
Treatment for candidiasis depends on the location and extent of the infection but usually involves antifungal medication.
- Topical antifungals – Ointments, creams, or vaginal pessaries containing clotrimazole or miconazole are commonly prescribed for skin or genital infections.
- Oral antifungals – Fluconazole and similar medications may be used for recurrent, widespread, or stubborn infections.
Invasive candidiasis requires intravenous antifungal therapy and close monitoring in a hospital setting.
Cost of Candidiasis Testing & Treatment in Singapore
At healthscreening.sg, we provide diagnostic and treatment services for candidiasis as part of our comprehensive women’s health.
| Test / Treatment | Test Type | Prices* |
|---|---|---|
| Consultation | From $49.05 | |
| Testing | ||
|
DNA Probe/Multiplex Real Time PCR for Vaginitis Gardnerella vaginalis, Candida albicans and Trichomonas vaginalis |
Swab | $147.15 |
|
Basic Female Genital Screen (5 tests) Chlamydia PCR, Gonorrhoea PCR, Candida, Gardnerella Vaginosis, Trichomonas |
Swab | $268 |
|
Enhanced Female Genital Screen (9 tests) Chlamydia, Gonorrhoea, Mycoplasma genitalium, Mycoplasma hominis, Trichomonas, Ureaplasma parvum, Ureaplasma urealyticum, Candida, Gardnerella Vaginosis |
Swab | $348 |
|
Complete Female STD Screen (15 tests) HIV, Syphilis, Hepatitis B, Hepatitis C, Herpes Simplex Virus 1 and 2, Chlamydia, Gonorrhoea, Mycoplasma genitalium, Mycoplasma hominis, Trichomonas, Ureaplasma parvum, Ureaplasma urealyticum, Candida, Gardnerella Vaginosis |
Blood + Swab | $478 |
| Treatment | ||
| Topical Antifungal Cream | From $10.90 | |
| Pessary Antifungal Cream | $59.95 for full course of treatment | |
| Oral Antifungal Medication | From $1.41 per tab | |
*Prices are NETT and inclusive of GST.
^Prices last updated on
Jan 28, 2026. While every effort is made to keep pricing information up to date, please contact our team to confirm the latest rates.
We offer private and confidential STI
testing, available as standalone tests or in comprehensive packages, along with treatment where
necessary. Male or female doctors are available upon request for your comfort, subject to availability.
For more information or to schedule an appointment, please contact
our clinic directly.
How Can Candidiasis Be Prevented?
Preventing candidiasis involves reducing the conditions that allow Candida to thrive and supporting a balanced microbiome. You can help prevent infections by:
- Maintaining good genital and skin hygiene.
- Choosing breathable, cotton-based clothing and keeping skin folds dry.
- Avoiding scented soaps, douches, or feminine sprays that disrupt the vagina’s natural flora.
- Using antibiotics only when medically necessary and following your doctor’s advice.
- Keeping blood sugar levels stable if you have diabetes.
Individuals who experience recurrent yeast infections may benefit from regular check-ups to identify and manage any underlying factors.

When Should You See a Doctor for Candidiasis?
You should consult a doctor if you experience symptoms that persist, worsen, or recur frequently. Seek medical advice if:
- Over-the-counter treatments do not relieve your symptoms.
- You experience repeated episodes of candidiasis.
- You develop fever, fatigue, or other signs that the infection may have spread.
- You have a medical condition that weakens your immune system.
How to Book an Appointment for Candidiasis Testing?
Why Choose Us?








Navigate Easy With Google Maps
Health Screening Singapore (Anson House)
Nearest MRT: EW15 Tanjong PagarHealth Screening Singapore (Camden Medical Centre)
Nearest MRT: TE13 Orchard BoulevardHealth Screening Singapore (CPF Jurong Building)
Nearest MRT: NS1/EW24 Jurong EastFrequently Asked Questions (FAQ)
Candidiasis is not classified as a sexually transmitted disease, but it can occasionally be transmitted between sexual partners. The infection results mainly from an overgrowth of Candida yeast that naturally lives on the body. However, sexual activity may sometimes contribute to its development or recurrence. If you or your partner experience persistent symptoms, it is advisable to consult a doctor for evaluation and appropriate treatment.
Candidiasis often causes itching, redness, and irritation in the affected area, with symptoms varying by site. Vaginal infections may produce thick white discharge and burning, while oral infections can cause white patches and soreness. Skin infections typically appear as red, itchy rashes. Because similar symptoms can occur with other conditions, it is advisable to see a doctor for accurate diagnosis and treatment.
Treatment for candidiasis usually involves antifungal medication, either topical or oral, depending on the infection’s severity and location. Common options include clotrimazole or miconazole creams for skin and vaginal infections, and fluconazole tablets for more extensive or recurrent cases. Severe or invasive infections require hospital-based treatment. If you are experiencing symptoms or suspect a candidiasis infection, it is advisable to consult a doctor for proper diagnosis and treatment.
Mild candidiasis often improves within a few days of starting antifungal treatment, while more persistent or widespread infections may take longer to clear. The speed of recovery depends on the infection site, overall health, and adherence to medication. Maintaining good hygiene, keeping affected areas dry, and avoiding irritants can help the healing process. Always follow your doctor’s prescribed treatment plan to support a smooth recovery.
Most forms of candidiasis are mild and treatable, but untreated or recurrent infections can lead to discomfort or complications. Invasive candidiasis, where the infection spreads to the bloodstream or internal organs, is uncommon but potentially life-threatening and requires immediate medical care. If your symptoms persist, worsen, or you suspect a candidiasis infection, it is advisable to consult a doctor for proper evaluation and treatment.
Candidiasis is neither a urinary tract infection nor a traditional sexually transmitted infection. It results from an overgrowth of Candida yeast, which normally lives harmlessly in the body. However, it may sometimes occur alongside UTIs or other infections, and sexual activity can occasionally contribute to its onset. If you are uncertain about your symptoms, it is best to seek medical assessment.
The main cause of candidiasis is an imbalance in the body’s normal microorganisms, allowing Candida to multiply excessively. This imbalance may be triggered by antibiotic use, hormonal changes, high blood sugar, poor hygiene, or weakened immunity. Although the infection is not always sexually transmitted, intimate contact can sometimes contribute to its recurrence. Managing underlying factors can help reduce the risk of infection.
Candidiasis can resolve with appropriate antifungal treatment, and mild cases may improve within a few days. However, untreated infections can persist or recur, especially if underlying factors such as poor hygiene, hormonal changes, or antibiotic use remain unaddressed. If symptoms do not improve with over-the-counter remedies or return frequently, it is advisable to consult a doctor for further evaluation and treatment.
Testing for Candida involves swab, microscopy, or culture tests depending on the affected area, such as the mouth, genitals, or skin. Blood tests may be required for suspected systemic infection. These tests help identify the presence and type of Candida species to guide treatment. If you experience persistent symptoms, it is best to consult a doctor for proper diagnosis and testing.
There is limited scientific evidence directly linking Candida overgrowth to weight gain. While some theories suggest that chronic fungal imbalance may influence metabolism or cravings, such associations remain unproven. Weight changes are more likely related to diet, hormones, or other health factors. If you suspect an underlying infection or experience unexplained weight changes, it is advisable to consult your doctor for assessment.
Candidiasis is not typically contagious but can occasionally spread through direct skin or sexual contact. It mainly develops when natural microorganisms in the body become imbalanced, allowing Candida to multiply. Sharing personal hygiene items or engaging in sexual activity during an active infection may increase the risk of transfer. Good hygiene and timely treatment help minimise spread and recurrence.
If left untreated, mild candidiasis may worsen or recur, causing greater irritation and inflammation. In rare cases, particularly in individuals with weakened immune systems, the infection can spread to the bloodstream or internal organs, leading to invasive candidiasis that requires urgent medical care. If you experience symptoms or suspect a Candida infection, it is advisable to seek medical evaluation promptly.
When managing candidiasis, it may help to reduce foods high in sugar and refined carbohydrates, as these can encourage yeast growth. Limiting alcohol and processed foods may also be beneficial. A balanced diet rich in vegetables, lean proteins, and whole grains supports immune and digestive health. It is best to consult your doctor for personalised dietary advice on managing Candida.
