Gardnerella Vaginalis: Symptoms, Causes, and Treatment Options
What Is Gardnerella Vaginalis?
Gardnerella vaginalis is a naturally occurring bacterium in the vaginal environment that
can lead to bacterial vaginosis (BV) when it multiplies excessively.
BV develops when the usual balance of bacteria in the vagina changes, allowing
Gardnerella and other bacteria to outnumber the protective lactobacilli that maintain acidity and
overall vaginal health. This imbalance can cause symptoms such as an unusual discharge or a
noticeable odour.
In some cases, untreated infections may increase the likelihood of
complications involving pregnancy or other reproductive health concerns.
What Are Causes of Gardnerella Vaginalis?
An overgrowth of Gardnerella vaginalis happens when the protective bacteria in the vagina
decline, creating conditions that allow Gardnerella and other bacteria to multiply.
Various biological, lifestyle, and environmental influences can trigger this shift.
Common factors that may contribute include:
- Engaging in unprotected sexual activity or having multiple sexual partners
- Taking antibiotics that disturb the vaginal microbiota
- Hormonal fluctuations during menstruation, pregnancy, or menopause
- Regular vaginal douching
Although not classified as a typical sexually transmitted infection (STI), BV is more frequent among sexually active individuals and can be linked to changes in sexual partners. However, it may still develop in those who are not currently sexually active.
What Are Symptoms of Gardnerella Vaginalis?
When Gardnerella vaginalis becomes dominant, it often results in bacterial vaginosis, which can present with several distinctive symptoms. These may include:
- A noticeable fish-like odour, particularly after sexual intercourse
- Vaginal discharge that is thin and grey or white in colour
- Itching, irritation, or general discomfort in the vaginal area
- A burning feeling when passing urine
Some women may experience no symptoms at all, especially when the imbalance is mild or newly developed, making regular check-ups important if BV is suspected.

What Are the Risks of Untreated Gardnerella Vaginalis?
If bacterial vaginosis caused by Gardnerella vaginalis is not treated, it can heighten the risk of several reproductive and general health issues.
- Increased vulnerability to STIs – A disrupted bacterial environment weakens natural defences, making infection by viruses and other bacteria more likely.
- Pregnancy complications – Untreated BV may increase the risk of preterm delivery or low birth weight due to inflammation of the reproductive tissues.
- Pelvic inflammatory disease (PID) – The bacteria may travel upwards into the uterus and fallopian tubes, potentially causing long-term inflammation and fertility problems.
- Post-surgical infections – Procedures involving the reproductive tract, such as intrauterine device (IUD) insertion or abortion, carry higher infection risks when the vaginal flora is imbalanced.
How Is Gardnerella Vaginalis Diagnosed?
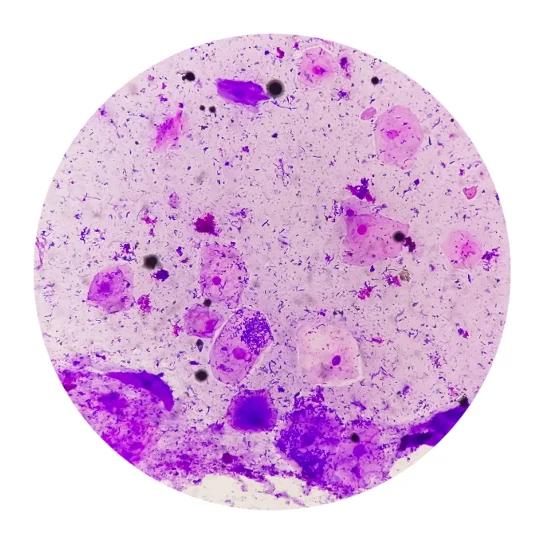
Diagnosis of Gardnerella vaginalis overgrowth usually involves evaluating symptoms alongside laboratory tests that confirm bacterial vaginosis. A vaginal swab is usually collected to evaluate bacterial balance through several testing methods.
- Microscopic examination – The sample is inspected for “clue cells,” which are vaginal cells coated with bacteria.
- pH testing – A pH higher than 4.5 suggests reduced vaginal acidity and an imbalance of bacteria.
- Whiff test – Adding a potassium hydroxide solution to the swab can release a fishy odour if BV is present.
- Nucleic acid amplification tests (NAATs) – These molecular tests detect bacterial DNA with high precision and are often used when more accurate identification is necessary.

What Is the Treatment for Gardnerella Vaginalis?
Treatment for Gardnerella vaginalis overgrowth focuses on restoring the natural bacterial
balance in the vagina using targeted antibiotics.
Metronidazole is typically prescribed, either taken orally or applied
intravaginally. Clindamycin may also be used, available
in both oral and topical formulations. For recurrent infections, probiotic supplementation can help
promote the growth of healthy vaginal bacteria.
Lifestyle adjustments may further reduce the likelihood of recurrence, and follow-up consultations are
useful for identifying possible contributing factors such as hygiene practices or sexual activity.
Cost of Gardnerella Vaginalis Testing & Treatment
At healthscreening.sg, we offer testing and treatment for bacterial vaginosis, including cases linked to Gardnerella vaginalis, with prices listed below.
| Test / Treatment | Test Type | Prices* |
|---|---|---|
| Consultation | From $49.05 | |
| Testing | ||
|
DNA Probe/Multiplex Real Time PCR for Vaginitis Gardnerella vaginalis, Candida albicans and Trichomonas vaginalis |
Swab | $147.15 |
|
Basic Female Genital Screen (5 tests) Chlamydia PCR, Gonorrhoea PCR, Candida, Gardnerella Vaginosis, Trichomonas |
Swab | $268 |
|
Enhanced Female Genital Screen (9 tests) Chlamydia, Gonorrhoea, Mycoplasma genitalium, Mycoplasma hominis, Trichomonas, Ureaplasma parvum, Ureaplasma urealyticum, Candida, Gardnerella Vaginosis |
Swab | $348 |
|
Complete Female STD Screen (15 tests) HIV, Syphilis, Hepatitis B, Hepatitis C, Herpes Simplex Virus 1 and 2, Chlamydia, Gonorrhoea, Mycoplasma genitalium, Mycoplasma hominis, Trichomonas, Ureaplasma parvum, Ureaplasma urealyticum, Candida, Gardnerella Vaginosis |
Blood + Swab | $478 |
| Treatment | ||
| Oral Antibiotics | From $0.87 per tab | |
| Intravaginal Antibiotics | $59.95 per box | |
*Prices are NETT and inclusive of GST.
We also provide a comprehensive range of STI
screening and women’s health
services. Female doctors are available upon request to ensure comfort and privacy during your
visit.
For more information or to book an appointment, please contact
us.
How to Prevent Gardnerella Vaginalis Overgrowth?
Maintaining a healthy vaginal environment is key to reducing the risk of Gardnerella vaginalis overgrowth. The following habits can help:
- Avoid vaginal douching, as it disrupts the natural bacterial balance.
- Use condoms during sexual activity to limit exposure to bacteria that may cause imbalance.
- Take prescribed antibiotics exactly as directed to prevent upsetting the natural balance of bacteria in the vagina.
- Wear breathable, cotton-based undergarments to maintain dryness and reduce irritation.
Book an Appointment for Gardnerella Vaginalis Testing
Why Choose Us?








Navigate Easy With Google Maps
Health Screening Singapore
(Anson House)
Health Screening Singapore
(Camden Medical Centre)
Frequently Asked Questions (FAQ)
A positive test for Gardnerella vaginalis indicates an overgrowth of this bacterium, often associated with bacterial vaginosis (BV). It does not necessarily mean you have a sexually transmitted infection, as G. vaginalis can exist naturally in the vagina. Treatment may be recommended by your doctor to restore bacterial balance and relieve symptoms.
Having Gardnerella vaginalis is not inherently harmful, as it can be part of the normal vaginal microbiota. However, when it multiplies excessively, it may lead to bacterial vaginosis (BV), which can cause discharge, odour, or discomfort. Untreated BV may increase the risk of complications such as pelvic infections or pregnancy-related issues. If symptoms occur or persist, or you suspect BV, it is advisable to seek medical evaluation for diagnosis and treatment.
No, Gardnerella vaginalis overgrowth causes bacterial vaginosis, not a yeast infection. BV results from an imbalance of vaginal bacteria, while yeast infections are caused by the overgrowth of fungi, typically Candida albicans. Though both may cause vaginal irritation or discharge, their treatments differ, as BV is usually managed with antibiotics to restore bacterial balance, while yeast infections are treated with antifungal medications to reduce fungal growth.
Gardnerella vaginalis is not considered a typical sexually transmitted infection. It can occur in both sexually active and inactive individuals, as it arises from changes in the natural vaginal microbiome rather than direct transmission. However, sexual activity, particularly with new or multiple partners, may increase the likelihood of bacterial imbalance and recurrence.
Yes, Gardnerella vaginalis overgrowth can resolve with appropriate antibiotic treatment, which helps restore healthy bacterial balance. In some cases, BV may recur, particularly if underlying factors such as hormonal changes or sexual activity contribute to imbalance. Maintaining good vaginal hygiene and completing prescribed treatment can reduce recurrence. If you experience symptoms or suspect BV caused by Gardnerella, it is advisable to seek medical evaluation and treatment.
Yes, a strong, fish-like odour is one of the most recognisable symptoms of bacterial vaginosis caused by Gardnerella vaginalis. The odour often becomes more noticeable after sexual intercourse due to changes in vaginal pH. While this symptom is common, some individuals may experience BV without any smell. If you notice persistent vaginal odour or discharge, it is best to consult a doctor for evaluation and treatment.
Gardnerella vaginalis does not directly cause urinary tract infections, but an overgrowth may irritate nearby tissues, leading to discomfort similar to UTI symptoms. Occasionally, bacteria from the vagina may spread to the urinary tract, increasing infection risk. If you experience pain during urination, frequent urination, or persistent irritation, it is advisable to see a doctor for proper diagnosis and treatment.
No, Gardnerella vaginalis and gonorrhoea are different infections caused by unrelated bacteria. G. vaginalis is linked to bacterial vaginosis, which develops when the normal vaginal bacteria become imbalanced, while gonorrhoea is a sexually transmitted infection (STI) caused by Neisseria gonorrhoeae. Although both may cause vaginal discharge or discomfort, their modes of transmission, underlying causes, and treatments differ significantly.
Gardnerella vaginalis and human papillomavirus (HPV) are not directly related, but bacterial vaginosis caused by G. vaginalis can make it easier for HPV and other viruses to infect the cervix by disrupting the natural vaginal barrier. Both conditions affect the genital tract but arise from different causes, as BV results from bacterial imbalance while HPV is a viral infection spread through sexual contact.
Bacterial vaginosis is not typically associated with itching, as it mainly causes abnormal discharge and a strong odour. However, mild irritation or discomfort can occasionally occur, especially if the vaginal pH is significantly altered. Persistent or severe itching is more commonly linked to yeast infections rather than BV. If you experience ongoing itchiness or discharge, it is advisable to see a doctor to confirm the cause and receive suitable treatment.
Yes, Gardnerella vaginalis overgrowth can cause a mild burning sensation, particularly during urination or sexual activity. This occurs when bacterial imbalance leads to inflammation or irritation of the vaginal tissue. The symptom may resemble that of a urinary tract or yeast infection, making proper diagnosis important. If you experience persistent burning or discomfort, it is best to consult a doctor for evaluation and treatment.
Bacterial vaginosis does not usually cause bleeding, but light spotting may sometimes occur due to irritation of the vaginal or cervical lining. Inflammation caused by BV can make these tissues more sensitive, especially after sexual intercourse. If you experience frequent or unexplained bleeding, it is important to see a doctor, as other gynaecological conditions may need to be ruled out through proper examination and testing.
Bacterial vaginosis itself rarely causes cramps, as it mainly affects the vaginal environment rather than the uterus. However, if BV leads to inflammation or spreads to the upper reproductive tract, it may contribute to pelvic discomfort or mild cramping. Persistent or severe cramps could indicate other conditions such as pelvic inflammatory disease (PID). If you experience ongoing pain or cramping, it is advisable to consult a doctor for further evaluation.
