What Is a Vaginal Yeast Infection?
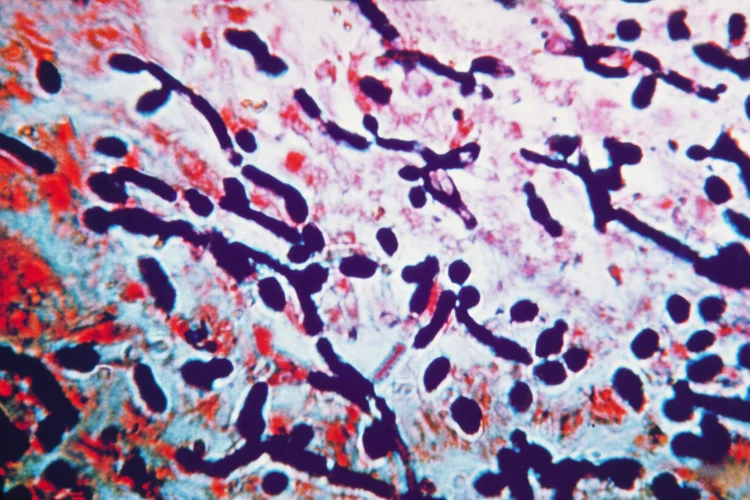
A vaginal yeast infection, also known as vaginal candidiasis or thrush, is a
common fungal infection that develops when yeast from the
Candida species multiplies excessively in the vaginal
area. Although Candida albicans naturally
exists in the vaginal microbiome, a disruption in the body's normal bacterial
balance can allow it to overgrow and cause infection.
The condition commonly produces symptoms such as vaginal itching, a burning
feeling, unusual discharge, and soreness around the vulva. These may interfere
with daily routines, rest, and sexual comfort.
While yeast infections are not classified as sexually transmitted infections (STIs),
friction during sexual activity or transfer of yeast between partners may
occasionally lead to flare-ups.

What Are Symptoms of Vaginal Yeast Infection?
A vaginal yeast infection typically presents with irritation and discharge, though the intensity and duration of symptoms can vary widely. Common indicators include:
- Persistent itching or irritation of the vulva and surrounding skin
- Thick, white discharge that looks similar to cottage cheese
- Redness or swelling in the vaginal area
- General soreness or discomfort, especially when walking or sitting
- Pain or a burning sensation when passing urine or during intercourse
For some, symptoms remain mild and short-lived, while for others they may be more disruptive and recurrent.
What Causes Vaginal Yeast Infection?
Vaginal yeast infections develop when the natural balance between bacteria and
fungi in the vagina is disrupted. Various biological and environmental triggers can
contribute to this imbalance.
Frequent causes include:
- Antibiotics – Broad-spectrum antibiotics can destroy beneficial bacteria that normally keep yeast growth under control.
- Hormonal changes – Fluctuations related to pregnancy, oral contraceptives, or hormone therapy can encourage fungal overgrowth.
- Scented or harsh products – Perfumed soaps, douches, and sprays may irritate vaginal tissue and upset its natural environment.
- Tight or synthetic clothing – Limited airflow and trapped moisture create a warm, damp environment ideal for yeast to grow.
- Sexual contact – Although not an STI, sexual activity can occasionally trigger symptoms or reintroduce yeast after treatment.
- Uncontrolled diabetes – Higher blood glucose levels can feed yeast and increase infection risk.
- Weakened immune function – People with compromised immunity, such as those with HIV or undergoing chemotherapy, are more vulnerable.
How Is Vaginal Yeast Infection Diagnosed?
Diagnosis of a vaginal yeast infection involves evaluating symptoms, inspecting the
affected area, and, when required, confirming the presence of Candida through
laboratory testing.
Typical diagnostic steps include:
- Reviewing recent medication use, medical history, or hormonal changes that may increase susceptibility to infection.
- Conducting a pelvic examination to check for signs of redness, inflammation, or abnormal discharge.
- Collecting a vaginal swab for microscopic or culture analysis to determine the fungal species involved.
Since symptoms can resemble those of bacterial vaginosis, trichomoniasis, or certain STIs, laboratory testing helps ensure that the most appropriate treatment is given.
How Is a Vaginal Yeast Infection Treated?
Vaginal yeast infections are generally treated with antifungal medicines, available as topical creams, pessaries, or oral tablets. The type and duration of treatment depend on how severe or frequent the infection is.
| Treatment Option | Description |
|---|---|
| Topical antifungal medications | Applied externally or inserted into the vagina to relieve symptoms and reduce fungal overgrowth. Common examples include clotrimazole and miconazole. |
| Oral antifungal tablets | Usually prescribed as a single-dose treatment for uncomplicated vaginal yeast infections. The most common option is fluconazole. |
| Combination therapy | Used for recurrent or severe infections, typically defined as four or more episodes within a 12-month period, and involves both topical and oral antifungal medication administered over an extended treatment course. |
| Managing contributing factors | Involves addressing blood sugar control, hormonal balance, or potential reinfection to reduce the risk of recurrence. |
Cost of Vaginal Yeast Infection Diagnosis & Treatment
At healthscreening.sg, diagnosis and treatment for vaginal yeast infections are available as part of our comprehensive women's health services.
| Test / Treatment | Test Type | Price* |
|---|---|---|
| Consultation | From $49.05 | |
| Testing | ||
|
DNA Probe/Multiplex Real Time PCR for Vaginitis Gardnerella vaginalis, Candida albicans and Trichomonas vaginalis |
Swab | $147.15 |
|
Basic Female Genital Screen (5 tests) Chlamydia PCR, Gonorrhoea PCR, Candida, Gardnerella Vaginosis, Trichomonas |
Swab | $268 |
|
Enhanced Female Genital Screen (9 tests) Chlamydia, Gonorrhoea, Mycoplasma genitalium, Mycoplasma hominis, Trichomonas, Ureaplasma parvum, Ureaplasma urealyticum, Candida, Gardnerella Vaginosis |
Swab | $348 |
|
Complete Female STD Screen (15 tests) HIV, Syphilis, Hepatitis B, Hepatitis C, Herpes Simplex Virus 1 and 2, Chlamydia, Gonorrhoea, Mycoplasma genitalium, Mycoplasma hominis, Trichomonas, Ureaplasma parvum, Ureaplasma urealyticum, Candida, Gardnerella Vaginosis |
Blood + Swab | $478 |
| Treatment | ||
| Topical Antifungal Cream | From $10.90 | |
| Pessary Antifungal Medication | $59.95 for full course of treatment | |
| Oral Antifungal Medication | From $1.41 per tab | |
*Prices are NETT and inclusive of GST.
^Prices last updated on
Jan 28, 2026. While every effort is made to keep pricing information up to date, please contact our team to confirm the latest rates.
We provide discreet and
confidential testing and treatment for STIs, which can be arranged as individual
tests or included within broader screening packages. To ensure your comfort and privacy,
you may request either a male or female doctor for your consultation.
For information on available tests, treatment options, or to book an appointment, please
contact
us directly.
How to Prevent a Vaginal Yeast Infection?
Reducing the risk of vaginal yeast infections involves maintaining a healthy vaginal environment and adopting habits that help preserve natural bacterial balance. Helpful preventive steps include:
- Using antibiotics only when medically necessary
- Avoiding perfumed soaps, wipes, or sprays that may irritate delicate tissue
- Keeping the genital area clean and dry without over-washing
- Wearing breathable cotton underwear and loose-fitting clothing
- Changing out of wet gym or swimwear promptly
- Maintaining good blood sugar control if you have diabetes
When Should You See a Doctor?
Medical assessment is advisable if you experience vaginal itching, discharge, or irritation that persists despite over-the-counter treatment. You should also seek care if:
- The discharge has an unusual colour or odour
- There is pelvic pain, fever, or bleeding unrelated to menstruation
- You have had multiple infections within a short time
- Symptoms return soon after treatment ends
A clinical review helps determine whether another infection or skin condition may be responsible for your symptoms and ensures that you receive the most suitable treatment.
How to Book an Appointment to Test for Vaginal Yeast Infection?
Navigate Easy With Google Maps
Health Screening Singapore (Anson House)
Nearest MRT: EW15 Tanjong PagarHealth Screening Singapore (Camden Medical Centre)
Nearest MRT: TE13 Orchard BoulevardHealth Screening Singapore (CPF Jurong Building)
Nearest MRT: NS1/EW24 Jurong EastFrequently Asked Questions (FAQ)
Yes, mild vaginal yeast infections can often be managed with over-the-counter antifungal creams, pessaries, or oral tablets available at pharmacies. However, as symptoms may resemble other vaginal infections, it is advisable to confirm the diagnosis before treatment, especially if symptoms are severe, recurrent, or do not improve after self-medication. If symptoms persist or worsen, it is best to consult a doctor for assessment and appropriate management.
Yes, a general practitioner (GP) can diagnose and treat vaginal yeast infections. A GP can perform an examination, recommend the most suitable antifungal medication, and identify any underlying factors such as antibiotic use, hormonal changes, or diabetes that may contribute to recurrence.
A mild yeast infection may sometimes improve with self-care and over-the-counter antifungal treatments, but untreated infections can worsen or recur. Relying on home remedies or waiting for symptoms to resolve naturally is not recommended, as similar symptoms can indicate other infections. If you are unsure of the cause, or symptoms persist after self-treatment, it is advisable to consult a doctor for evaluation and guidance.
While symptoms such as itching, thick white discharge, and irritation may suggest a yeast infection, only a vaginal swab test can confirm it. Because other conditions like bacterial vaginosis or sexually transmitted infections (STIs) can cause similar symptoms, it is best to consult your doctor for proper diagnosis and appropriate treatment.
Bacterial vaginosis, trichomoniasis, and some sexually transmitted infections (STIs) are often mistaken for yeast infections because they can cause discharge, itching, or irritation. Certain skin conditions, such as eczema or contact dermatitis around the vulva, may also appear similar. As these conditions require different treatments, it is advisable to seek medical evaluation for persistent or recurring symptoms.
A vaginal yeast infection occurs when the natural balance of bacteria and fungi in the vagina is disrupted, allowing Candida to overgrow. Common triggers include antibiotic use, hormonal changes, excessive moisture, or irritation from scented products. High blood sugar and weakened immunity may also increase susceptibility. If infections occur frequently or after medication use, it is advisable to discuss possible underlying causes with your doctor.
A mild vaginal yeast infection usually lasts three to seven days with appropriate antifungal treatment, while untreated or recurrent cases may persist longer. The duration can vary depending on factors such as overall health, use of antibiotics, or blood sugar control. If symptoms do not improve after a week of treatment or return frequently, it is advisable to consult your doctor for further evaluation and tailored management.
When managing a yeast infection, gently wash the external genital area with warm water and mild, unscented soap once daily, avoiding douches, scented wipes, or sprays that may irritate delicate tissue. Wearing breathable cotton undergarment and keeping the area dry also helps relieve discomfort. Over-washing or using harsh products may worsen irritation. If symptoms persist or worsen despite proper hygiene, it is best to consult a doctor.
Yes, a vaginal yeast infection can sometimes cause a burning sensation during urination, which may resemble a urinary tract infection (UTI). However, a UTI typically causes frequent urination, urgency, and cloudy urine, while a yeast infection often involves itching and thick discharge. Because symptoms may overlap, it is advisable to consult a doctor or undergo testing to confirm the diagnosis before starting treatment.
If left untreated, a vaginal yeast infection may worsen, causing increased itching, redness, swelling, and persistent discomfort. In some cases, it can lead to recurring infections or skin breakdown due to scratching. Although not life-threatening, untreated infections can significantly affect quality of life. If you suspect a yeast infection or experience persistent symptoms, it is advisable to seek medical evaluation for appropriate treatment.
Typical signs of a vaginal yeast infection include intense itching, redness, swelling, and a thick white discharge that resembles cottage cheese. A mild burning sensation may also occur during urination or intercourse. However, similar symptoms can occur with bacterial vaginosis or other infections. To confirm the cause and receive suitable treatment, it is advisable to visit a doctor for a pelvic examination or vaginal swab test.
A mild vaginal yeast infection may sometimes resolve naturally, but most require antifungal treatment to clear completely and prevent recurrence. Without treatment, symptoms such as itching and discharge may persist or worsen. Since similar symptoms can occur with other infections, it is advisable to confirm the diagnosis and seek medical care if symptoms continue beyond a few days or recur frequently.
A vaginal yeast infection is usually treated with antifungal medication available as creams, pessaries, or oral tablets. The choice of treatment depends on the severity and frequency of the infection. Maintaining good hygiene and avoiding scented products or tight clothing can also support recovery. If symptoms persist, recur, or worsen after treatment, it is best to consult a doctor for further evaluation.
Common signs of a vaginal yeast infection include itching or irritation around the vulva, thick white discharge resembling cottage cheese, redness or swelling of the vaginal area, and burning or soreness during urination or intercourse. These symptoms can range from mild to intense and may sometimes resemble other vaginal infections. If you notice these changes, it is advisable to seek medical assessment for confirmation and treatment.
When managing a yeast infection, avoid douching, using scented soaps or feminine sprays, or wearing tight synthetic clothing, as these can irritate the area and worsen symptoms. Refrain from scratching, which may cause further irritation or infection. It is also best to avoid sexual activity until symptoms resolve to prevent discomfort and possible recurrence. Always follow your doctor's advice regarding treatment and hygiene.
Yeast infections typically cause itching, redness, and thick white discharge, while bacterial vaginosis often leads to a thin, grey discharge with a noticeable odour. Because these conditions may appear similar, a vaginal swab or pH test is needed to confirm the diagnosis. If you are uncertain which infection you have, it is advisable to see a doctor for proper testing and treatment.
Women who use antibiotics, are pregnant, have diabetes, or experience hormonal changes are more prone to yeast infections. Those with weakened immune systems or who frequently use scented hygiene products may also be at higher risk. Although yeast infections are common and not sexually transmitted, managing underlying health factors can reduce recurrence. It is advisable to consult a doctor if infections occur often.
Stress itself does not directly cause a yeast infection, but chronic stress can weaken the immune system and make the body more susceptible to fungal overgrowth. Stress may also influence hormone balance and lifestyle habits, which can contribute to infection risk. Managing stress through adequate rest, balanced nutrition, and regular exercise may help support vaginal health. If symptoms develop, consult your doctor for a proper assessment.
